
Imagine a world where a seemingly run-of-the-mill infection, like a UTI or strep throat, comes with a deadly prognosis.
This grim existence may be our reality in the not-too-distant future. This is because some bacteria are resistant to the antibiotics we use to treat infections, rendering once-powerful drugs ineffective.
And the overprescription of antibiotics has sped up the rate at which bacteria are becoming resistant to any known cure. At this pace, by 2050 ten million people may die every year due to antibiotic-resistant infections.
If you haven’t yet heard about this global health threat, it’s time to take heed. Read on to learn more about antibiotic resistance and what we can do to try to change the trajectory of the future.
The discovery of penicillin, the world’s first antibiotic, marked a transitional time for modern medicine. This new “miracle” drug, discovered by chance, provided doctors with the ability to cure many deadly infections. Antibiotics have been helping people get well ever since.
But, like many success stories, there’s a concerning subplot – one that’s becoming more urgent than ever.
Alongside the increased use of antibiotics, the medical world has seen a growing number of infections that have developed antibiotic resistance. This occurs when bacteria adapt to resist the medications we use to fight them.
Germs (bacteria, viruses, fungi, etc.) adapt through genetic mutation to survive. The more exposure germs have to medication, the more likely a genetic mutation will occur to allow for survival against that medication. These surviving germs multiply, filling the world with even more resistant germs.
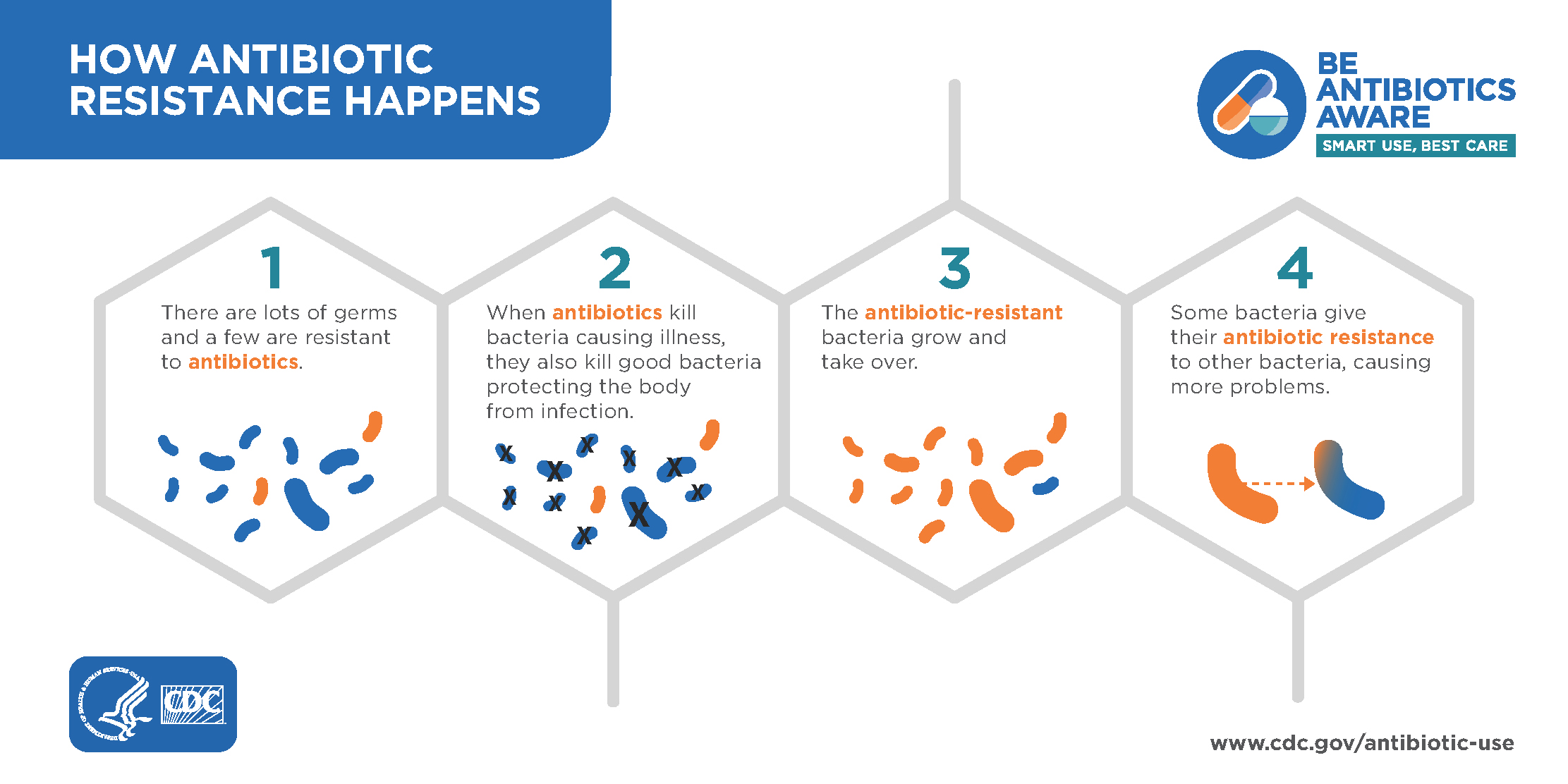
So, the more antibiotics we use, the faster bacteria “learn” to resist.
And unfortunately for us, the discovery of new antibiotics is outpaced by the rate at which antibiotic-resistant infections are growing. We aren’t able to keep up, which is why more and more people are dying from drug-resistant infectious diseases every year.
Of course, antibiotics are sometimes still the best way to fight certain types of infection. The effective use of antibiotics include:
Many bacterial sinus infections and ear infections won’t require antibiotics. In these cases, your doctor would opt to let your body heal on its own.
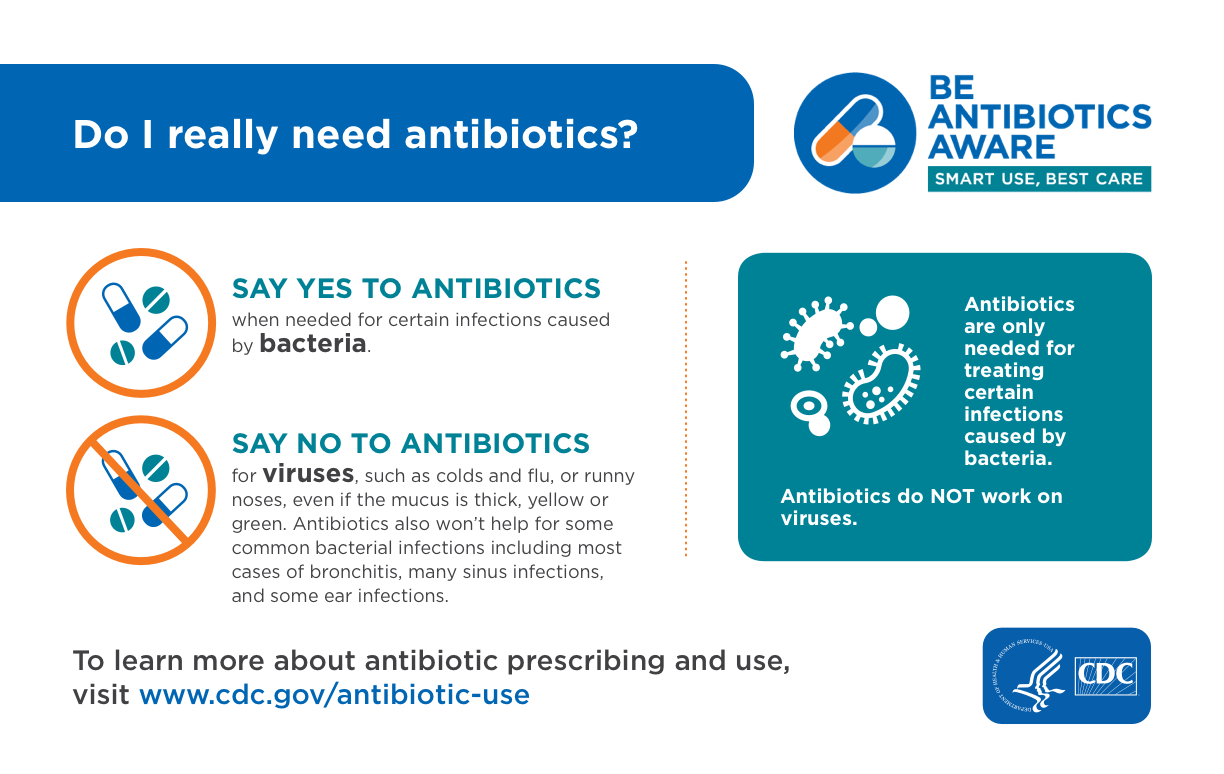
Antibiotics only help your body fight bacteria, and viral infections are not caused by bacteria. This means antibiotics will not cure viral upper-respiratory infections, like cold, flu, and yes, COVID-19. This is because they are viral infections, not bacterial. A medical professional can help you determine if your symptoms are a result of a viral or bacterial infection, and help recommend the best treatment.
In addition to the global public health concern of antibiotic resistance which, as described above, could have serious health consequences for each of us individually, using antibiotics can also have many other adverse physical effects on individuals. These can include:
These are yet another reason to take the use of antibiotics seriously and strive to make the best decision for every situation.
At the core of antibiotic stewardship is the idea of taking special care to only prescribe antibiotics when necessary. We now recognize that many illnesses for which many antibiotic prescriptions were provided in the past are either viral infections (which will not respond to antibiotics) or bacterial infections that will resolve on their own without antibiotic treatment. This set of facts coupled with greater knowledge of the potential harms of their use are what animates the concept of antibiotic stewardship.
The Centers for Disease Control and Prevention states that 30% of antibiotic prescriptions in the US are not needed. This can happen even more frequently in urgent care facilities when patients arrive requesting antibiotics and the clinician may not have access to a full health history of antibiotic use. While a patient might prefer a clinician to prescribe antibiotics to “cover all bases”, this may not be in the best interest of the patient’s safety and overall health.
Antibiotic Stewardship practices apply to clinicians, patients, and healthcare systems. By working together, we can all help fight the over-prescription of antibiotics and, in turn, reduce the rate at which antibiotic-resistant infections are growing.
Health care providers need to shoulder a large part of the responsibility in the battle against antibiotic resistance. However, there are steps that individuals like you can take to join in the fight. Some of these include:
Antibiotic stewardship is an important part of vybe’s mission. But remember—antibiotics are sometimes still the best answer for bacterial infections. If you suspect you’re sick, visit your local vybe urgent care for first-rate treatment centered on what’s best for you.
FIND YOUR VYBE